Top Facts
- Depression is more common in elderly people who also have other illnesses (such as heart disease or cancer) or whose function becomes limited. This is essential to note, as 80% of older adults have at least one chronic health condition, and 50% have two or more. (CDC)
- Among older adults, insomnia is a major risk factor for both onset and persistence of depression.
- Depression can look different depending on your culture. People from different cultures may experience mood disorders like depression in different ways. In some cultures, depression may be expressed in the form of physical symptoms, such as aches or pains, headaches, cramps, or digestive problems.
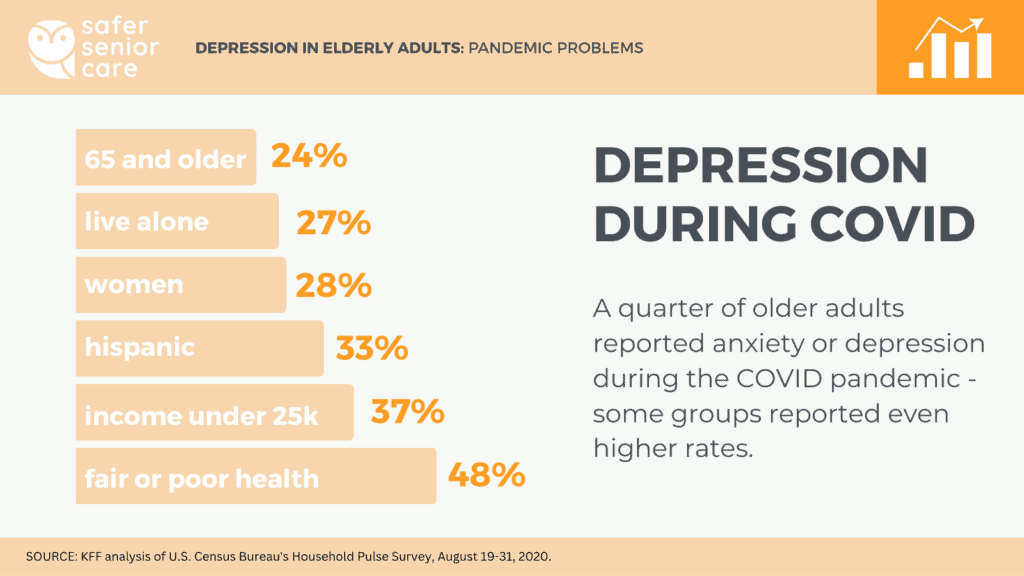
- 24% of adults ages 65 and older reported anxiety or depression in 2020. This is much higher than the 11% of older adults who reported depression or anxiety in 2018. However, older adults reported less anxiety or depression in 2020 than the 40% of younger adults under the age of 65 did. (Koma, 2020)
- Older people with depressive disorder have a 40% greater chance of premature death than their counterparts. (Zenebe 2021)
- Depression was undiagnosed in about 50% of cases, as found in one study (Zenebe 2021). This is likely due to the fact that depression often manifests itself differently in seniors than in younger adults, often with more physical symptoms. For example, fatigue can be erroneously attributed to old age. Additionally, the cognitive changes associated with untreated depression are often mistaken for dementia.
- Depression is especially dangerous for older adults. Late-life depression is associated with an increased risk of morbidity, increased risk of suicide, and greater self-neglect (Blazer, 2003)
- Seniors can experience various types of depression, including substance/medication-induced depression, depression to a medical condition, psychotic depression, postmenopausal depression, and seasonal affective disorder, among others. (NIA)
- Loneliness and social isolation are associated with higher rates of depression, making elderly seniors especially vulnerable, with less social interaction commonly the results of mobility issues or physical impairments. (NIA)
- Depression is common in people with Alzheimer’s and other forms of dementia. Dementia can cause some of the same symptoms as depression, and depression can be an early warning sign of possible dementia. (NIA)
- Women are more likely to report suffering from anxiety or depression than men. 28% of older women report suffering from anxiety or depression, vs. only 20% of men. (Koma, 2020)
- Suicide among older adults is more likely to be associated with depression than suicide at any other age (Conwell & Brent, 1996).
Who Gets Depressed?
- Depression is more common in those who suffer from poor health. 48% of older adults in poor or fair health reported anxiety or depression. Of older adults with good health, only 24% reported anxiety or depression, and just 14% of those in excellent or very good health. (Koma, 2020)
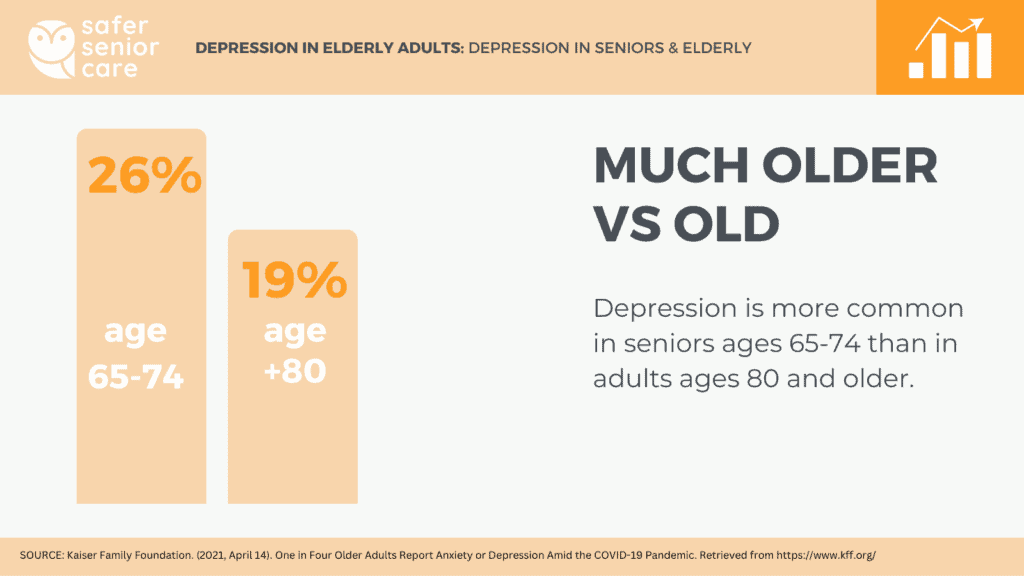
- Depression seems less common in the very old than the moderately old. 26% of adults ages 65-74 reported feelings of anxiety or depression compared to 19% of adults ages 80 and older. (Koma, 2020)
- Older adults with lower incomes deal more with depression. 37% of older adults with household incomes under $25,000 reported anxiety or depression – nearly 2x the rate (20%) among older adults with incomes exceeding $100,000 annually. (Koma, 2020)
- Past experience with depression can increase your risk. If you’ve experienced depression as a younger person, you may be more likely to have depression as an older adult. (NIA)
- 13.5% of elderly seniors who require home healthcare suffer from depression. Meanwhile, only 1-5% of elderly seniors suffer depression when living in a community setting. (Bruce, 2002)
- Late life depression is often the result of a combination of factors, including genetic vulnerabilities, cognitive decline, and stressful events that occur later in life – such as losing a partner. (Fiske, 2010)
- More than 50% of depressed older adults had the first episode after age 60. This further supports the idea that depression in older adults is often connected with stressful life events that occur later in life. (Fiske, 2010)
- One study found that depressive symptoms may be more common among Hispanic older women than non-Hispanic whites (Swenson, 2000)
- Rates of depression appear to be higher in older women than in older men (Djernes, 2006)
- Older adults in long-term care facilities experience the highest rates of depression, with up to 35% of residents experiencing depression symptoms. (Blazer, 2003)
- Bereavement triples a senior’s risk of depression – the largest effect size of any risk factors examined (Cole & Dendukuri, 2003).
- Men are more likely to become depressed following loss of a spouse than women are, and are more likely to remain depressed longer. (Umberson, 1992).
- Depression is more prevalent in developing countries, with 40% reporting depression in developing countries vs 17% in developed countries.(Zenebe 2021)
- Illinois is reported to be the least-depressing state for seniors, with only 8.2% of seniors experiencing depression, as opposed to Washington, the state with the highest reported number of depressed seniors at 20%. (CDC)
Statistics on Treating Depression in Elderly Adults
- Depression in late life is treatable, even among older adults with dementia. Behavioral therapy, cognitive behavioral therapy, cognitive bibliotherapy, problem-solving therapy, brief psychodynamic therapy, and life review/reminiscence therapy are effective but too infrequently used with older adults. (Fiske, 2010)
- There are programs to help. PEARLS (Program to Encourage Active, Rewarding Lives) is a treatment program designed to reduce symptoms of depression and improve quality of life among older adults. More than 50 sites in 18 states use PEARLS with great success. A University of Washington study determined that PEARLS participants had a 50% or higher reduction in symptoms of depression. (Ciechanowski, 2010)
- A large proportion of older adults with depression do not receive treatment of any kind, possibly due in part to the fact that depressed older adults are more likely to seek care from a primary care provider than a mental health specialist (Blazer, 2005).
- Medical costs are up to 51% higher among older adults with major depression than among those without depression. (Katon, 2003)
How Depression Looks Different Between Older and Younger Adults
- Depression looks different in older adults vs younger adults. Older adults are more likely to display cognitive changes, somatic symptoms, and loss of interest than younger adults are. (Fiske, 2010)
- Older adults are less likely to experience cognitive-affective symptoms of depression, including dysphoria and worthlessness/guilt, than are younger adults (Gallo et al., 1994)
- Sleep disturbance, fatigue, psychomotor retardation, loss of interest in living, and hopelessness about the future may be more prevalent in late-life depression than in depression in younger or middle-aged adults (Christensen et al., 1999).
- Older adults are less reactive to stressors, particularly those of an interpersonal nature, than younger adults (Neupert, 2007)
- Late onset depression in seniors is more likely to be related to dementia or a biological or psychological response to the events that are more common in late life (e.g., physical illness, bereavement, caregiving), where as early-onset depression is more often influenced by genes for depression. (Fiske, 2010)
- Religious involvement may also reduce the risk of depression in seniors, which is more frequently practiced by older adults than other age groups, (George, Ellison & Larson, 2002).
Depression and Connection With Other Illnesses and Disease
Depression in elderly seniors is often exacerbated or even triggered by other health issues or chronic diseases.
- 15% of senior patients with Type II diabetes suffer from major depression (Li, Ford, Strine, & Mokdad, 2008).
- 40% of individuals with late onset major depression with cognitive impairment develop dementia within three to five years (Alexopoulos, 2005; Schweitzer et al., 2002).
- 20-25% of stroke patients experience major depression (Park et al., 2007)
- 15-20% of those with Parkinson Disease experience major depression (Park et al., 2007)
- Only 22% of the depressed elderly seniors were found to take antidepressants to help with treatment. (Bruce, 2002)
- One study of the elderly Indian population found 21.7% of elderly individuals 60 and above experienced depressive disorders. (Barua, 2010)
- Vascular risk factors were associated with distinct depression symptom profiles, with sleep disturbance, psychomotor change, and loss of energy (Naarding, 2005)
- Inflammatory risk factors were associated with depression symptoms including appetite and sleep disturbance, loss of energy, concentration disturbance, and thoughts of death (Naarding, 2005)
- Depressed older women report more appetite disturbance than men, whereas older men report more agitation (Kockler & Heun, 2002)
How Sleep and Depression Relate for Elderly Seniors
- While previously associated as a symptom of depression, more recent studies have recently shown that insomnia often precedes the onset of depression in seniors (Perlis et al., 2006).
- Insomnia becomes more common with age, affecting 25% of older men and as much as 40% for women in their 80s (Lichstein, 2006).
Anxiety’s Connect to Depression in Elderly Adults
- 50% of older adults with depression also experience anxiety disorders (Beekman et al., 2000; Lenze et al., 2000).
- Late life depression is more severe, persistent, and difficult to treat when combined with anxiety (e.g., Andreescu et al., 2007; Schoevers et al., 2003).
- Rates of suicide are higher in older adults with anxiety and depression than in those with depression alone (Jeste, Hays, & Steffens, 2006; Schoevers et al., 2003).
- Anxiety may increase the risk of cognitive decline among older adults with treated depression (DeLuca et al., 2005).
What percentage of elderly suffer from depression?
Studies have shown that only 1-5% of elderly seniors suffer depression when living in a community setting. However, the rate jumps to 13.5% for those who require home healthcare.
What is the most common cause of depression in older adults?
There is no single cause for depression in older adults, but seniors have several unique depression risk factors, including chronic health conditions, reduced mobility, chronic pain, financial strain, elder abuse, caregiver stress, lack of physical activity, loneliness, and social isolation.
Is depression more prevalent in old age?
No – in fact, studies have shown that depression is less common later in life than it is in midlife or with young adults. However, late life depression is often more severe. Biological risk factors (such as a chronic illness) become much more prevalent in late life, as do certain life events (ex. Losing a partner, reduced mobility), whereas psychological vulnerability decreases and psychological resilience increases later in life.

